Food Insecurity Screening in the Allergy Specialty
Research and guidance to increase food insecurity knowledge and prevention
Food Allergies and Food Insecurity: Interlocking Challenges
Almost 1 in 13 American children (7.6%) have IgE-mediated food allergies (FA). The standard treatment for FA is avoiding allergenic foods, but alternative items can be hard to find and afford. Around 21% of children with FA also experience food insecurity (FI), or a household’s inability to acquire food due to lack of money or resources.
FI disproportionately affects Latinx, Native American and Black communities and has been rising during the pandemic. The impacts of FI on children include higher rates of asthma, obesity, academic trouble, behavior issues, anxiety, depression and more. The combination of FA and FI is dangerous: Children with both FI and FA are at greater risk of anaphylaxis than are their peers.
Shroba Heads AAAAI Food Insecurity Work Group
Because of the increase in FI, the American Academy of Allergy, Asthma and Immunology (AAAAI) FI Work Group surveyed allergists’ FI knowledge and practices. The survey report was published January 2022 in The Journal of Allergy and Clinical Immunology: In Practice.1
Jodi Shroba, APRN, MSN, CPNP, is the lead author and chair of the AAAAI FI Work Group. Her FI experience includes serving on the Children’s Mercy Hunger-Free Hospital Council and the medical advisory board of the Food Equality Initiative.
Food Insecurity Knowledge and Screening
In the fall of 2020, the work group surveyed a random sample of AAAAI members. COVID-19 fatigue may have played a part in the survey’s low response rate (6.3%), but it’s possible that lack of FI knowledge kept members from responding. If so, the survey may overestimate the FI knowledge base. Most respondents were allergists, female and white and worked in urban or suburban areas. The lack of diversity in the respondent sample may also skew results, especially because FI has had a greater impact on underrepresented communities.
The survey found 71.2% of respondents didn’t know if their FA patients experienced FI within the past six months. Only 24.5% routinely screened for FI. According to recent research, this suggests that fewer allergists screen for FI than do physician practices (30%) and hospitals (40%).2 Sixty-six percent of respondents were aware of general food banks in their area, but only 5.7% knew of allergen-free pantries, and 28.3% reported not being aware of any available FI resources.
Barriers to Screening
The most common barrier to FI screening was lack of knowledge (70%), followed by not having resources to give food-insecure patients (40%). It is also possible that FI assumptions keep allergists from screening: 27.8% said they didn’t think FI was an issue for their patients, and 63.9% reported their patients have never discussed struggling to afford safe foods.
Sixty percent of respondents were interested in implementing FI screenings. They requested logistical support — FI conversation tips and validated screening questionnaires — and FI resources, like pantry lists, pamphlets and digital materials.
Guidance on Implementing Screening
Responding to this interest, the work group offered the following FI screening advice:
- Prepare: Learn about FI. In addition to its own report, the group recommends the FI toolkit from the American Academy of Pediatrics (AAP).3
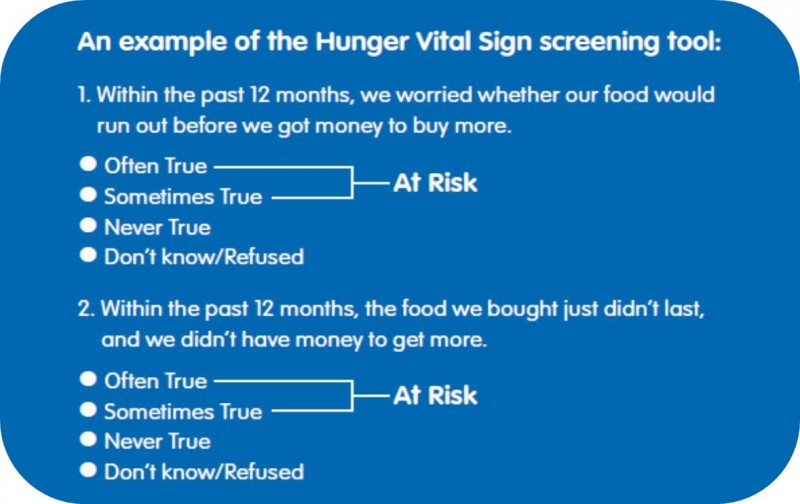
- Select a screening tool and method: Annual, universal screening will decrease provider bias and stigma. The most validated clinical screening tool is the Hunger Vital Sign (see below).
- Gather resources: Compile FI resources and highlight FA-sensitive ones. (See the full study for a starter list.) Federal FI programs include the Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and the Emergency Food Assistance Program, but none have specific provisions for families with FA.
- Get Involved: Create or join an FI group. For example, the Children’s Mercy Hunger-Free Hospital Council (HFHC) is a multidisciplinary team that works to improve the health care system’s response to FI, which is consistently identified as a priority issue in the hospital’s community health needs assessment. Initiatives supported by the HFHC include the Kids Eat Free summer food service program, fresh produce distribution and the community garden. Representation from the FA community lends a valuable perspective to the council, helping to ensure that programs to address FI are inclusive and equitable.
Future Areas of Study
More research is needed to understand the impact of FI on FA patients. Because FI has a greater impact on Latinx, Native American and Black communities, the work group would like to see increased diversity in FI and FA study samples. Future studies could include the impact of socioeconomic status on FA, whether specific FAs could be red flags for FI, and whether adding an FA question to the current Hunger Vital Sign tool would be helpful.
Learn more about food allergies and food insecurity

Jodi Shroba, MSN, APRN, CPNP
Food Allergy Program Coordinator, Allergy, Asthma and Immunology
jashroba@cmh.edu
(816) 960-8885
For consults, admissions or transport call: 1 (800) GO MERCY / 1 (800) 466-3729.
References:
1. Shroba J, Das R, Bilaver L, et al. Food insecurity in the food allergic population: a work group report of the AAAAI Adverse Reactions to Foods Committee. J Allergy Clin Immunol Pract. 2022;10(1):81-90. doi:10.1016/j.jaip.2021.10.058
2. Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw Open. 2019;2(9):e1911514. Published 2019 Sep 4. doi:10.1001/jamanetworkopen.2019.11514
3. Screen and Intervene: A Toolkit for Pediatricians to Address Food Insecurity. Developed by the American Academy of Pediatrics (AAP) and the Food Research & Action Center (FRAC). January 2021.
Children’s Mercy Kansas City is an independent, non-profit, 390-bed pediatric health system, providing over half a million patient encounters each year for children from across the country. Children’s Mercy is ranked by U.S. News & World Report in all ten specialties. We have received Magnet® recognition five times for excellence in nursing services. In affiliation with the University of Missouri-Kansas City, our faculty of nearly 800 pediatric specialists and researchers is actively involved in clinical care, pediatric research and educating the next generation of pediatricians and pediatric subspecialists. The Children’s Mercy Research Institute (CMRI) integrates research and clinical care with nationally recognized expertise in genomic medicine, precision therapeutics, population health, health care innovation and emerging infections. In 2021 the CMRI moved into a nine-story, 375,000-square-foot space emphasizing a translational approach to research in which clinicians and researchers work together to accelerate the pace of discovery that enhances care.
